
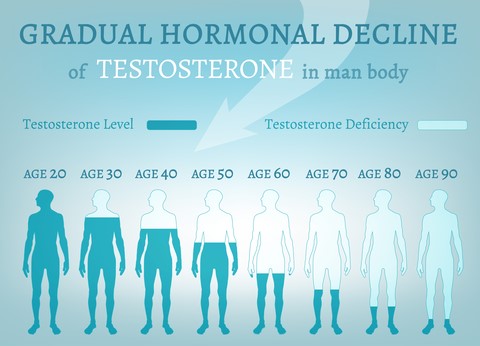
Andropause, also known as “male menopause,” is a term used to describe the age-related decline in testosterone levels in men. Testosterone levels decline about 1-2% each year starting in your early-30s. Unlike menopause in women, which can occur abruptly, andropause is a gradual process that typically begins around age 40. The symptoms of andropause can vary from person to person but often include poor concentration, decreased motivation, fatigue, loss of libido, erectile dysfunction, depression, weight gain, and decreased muscle mass. These symptoms can greatly impact a man’s quality of life and overall well-being.
By addressing hormone imbalances through hormone optimization, men can experience improvements in their energy levels, sexual function, cognitive abilities, mood, and overall quality of life.
Low testosterone is diagnosed through a blood test where physicians look for the level of testosterone, free testosterone, sex hormone binding globulin (SHBG,) and pituitary hormones important in male hormone production. Other tests may be conducted that may be impacted by testosterone therapy, such as cholesterol levels, and prostate specific antigen (PSA) levels.
Hormone optimization in men involves the process of optimizing various hormone levels to support overall health and well-being. Hormones are important chemical messengers that regulate various bodily functions, including metabolism, sexual function, muscle growth, mood, and cognition.
In men, the primary focus of hormone optimization is on testosterone, estrogen, and sometimes other hormones like thyroid hormones. Testosterone is the main male sex hormone and plays a crucial role in maintaining muscle mass, bone density, sperm production, libido, and energy levels. Estrogen, often associated with females, is also present in men and is essential for bone health and mood regulation.
To optimize hormones in men, blood tests are conducted to evaluate hormone levels and identify any imbalances or deficiencies. If hormone levels are found to be outside the normal range or if symptoms of hormone deficiency are present, hormone replacement therapy (HRT) may be recommended.
Hormone replacement therapy (HRT) can be carried out using either synthetic hormones or bioidentical hormones, which closely resemble the hormones naturally produced by the body. For men with low testosterone levels, a common form of HRT is testosterone replacement therapy (TRT). TRT can be administered through various methods such as injections, transdermal patches, gels, or pellets inserted under the skin.
The goal of hormone optimization in men is to bring hormone levels back to a healthy range, relieve symptoms associated with hormone deficiencies, and enhance overall quality of life. It is crucial to emphasize that hormone optimization should be conducted under the guidance and supervision of a qualified healthcare professional to ensure both safety and effectiveness of treatment.
Testosterone replacement therapy (TRT) can be administered in many forms.
Injection therapy is a common and effective option. There is a lot of flexibility with injection therapy as your physician can alter the dose and schedule of injections to maximize your testosterone levels. Unlike with topical testosterone treatments, there is no risk of accidently transferring testosterone to your spouse or children through skin contact. And, unlike with some oral testosterone treatments, there is no no concern for damaging the liver. It is a very effective therapy, but it does require the patient or patient’s partner to learn how to inject or make frequent office visits.
There are several transdermal (TD), or topical, forms of testosterone treatment. The most common form is a gel that is applied to clean, dry skin every day at the same time, usually after a man gets out of the shower. TD application is easy, well-tolerated and allows for good absorption of testosterone and an even delivery of the hormone throughout the day. There are minimal side effects. Some men will have a mild skin irritation while others may see an increase in their hematocrit, which will then need to be monitored. Men on TD therapy do need to be careful not to have skin to skin contact with other individuals until the application site is washed. Most products absorb after 2 hours of skin contact so washing the area after 2 hours provides the safest way to avoid transmission of active testosterone to others.
Once starting TRT, patients should notice improved energy levels, exercise tolerance, libido and erectile function within the first few weeks of therapy. Long term results may include weight loss, especially when combined with a vigorous exercise and nutrition regimen. Optimal results will be achieved within about three to six months. Periodic symptom and blood monitoring is essential to good therapeutic response. Once your R&R Rejuvenation physician has you on a stable dosing regimen, bloodwork will be checked every 6 months or so to ensure safety.
Short term side effects of testosterone replacement therapy may include:
Long term TRT side effects are known to be more problematic, including the possible risk of:
A controversial issue in prescribing TRT to aging healthy men is that once a person begins to take it, the body will stop making testosterone. This makes a person dependent on taking the hormone replacement long-term.
TRT may not be recommended when a person has conditions such as:
If you are consider starting hormone optimization therapy or have more questions, reach out at R&R Rejuvenation to have a free consultation with Dr. Kim. Either call 937-802-3151 or email at DrKim@RandRRejuvenation.com today.
